Restorative Prosthetics and Orthotics
We Treat the Patient, Not the Claim.
or
Our Services
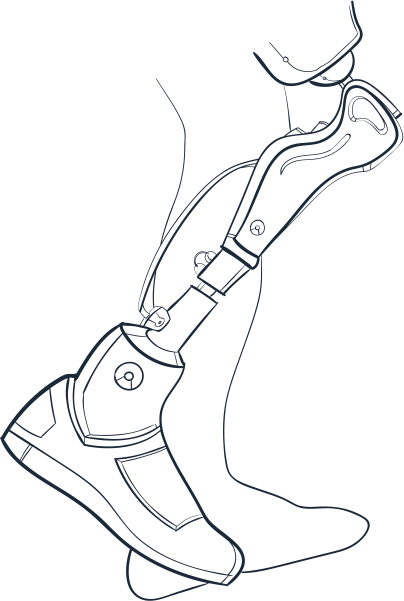
Prosthetics
All our prosthetic devices are made using the latest technology and tools in the industry.
Orthotics
We offer custom support and bracing solutions designed to assist you to move freely and live better.

Pediatrics
Our pediatric specialists offer high-quality, individualized care that you can rely on.
Cranial Helmets
Cranial helmet therapy is a procedure that’s normally prescribed to assist in molding the baby’s skull into perfect shape
O&P Technology
Our Orthotics and Prosthetics specialists combine skills coming from technology, science and art to fabricate, evaluate and fit orthopedic braces.

Advanced Technology
Our highly trained technicians and clinicians combine digital carvers, 3D printers and optical scanners to maximize the function and fit of your prosthesis.

Aaron Sorensen, MBA, CPO, LPO
Chief Executive Officer
About
Restorative Prosthetics and Orthotics
Restorative Health Services Group is one of Middle Tennessee’s leading providers of best prosthetic and orthotic care. It is a privately held company, driven by the unwavering dedication of its founder and president, Aaron Sorensen and his team.
As both the owner and a skilled clinician, Aaron treats a lot of patients daily. Our expertise and dedication can assist you in regaining your independence and doing the activities you love.

Lauren Vaughn
Executive Vice President of Operations
Restorative Group Community




Our Goals
From simple to extraordinary, Restorative Health Services Group is here to assist you in pursuing the things you love. Our goal is to offer the best prosthetic and orthotic care to the communities we diligently serve.

Helping patients regain their mobility

Focused on Patients’ Outcome

Quality prosthetic and orthotic care

Proper use of cutting-edge technology
Find Your Restorative Location
Patient Resources
Click on the Restorative Location Near You
With locations across Middle Tennessee, we offer convenient prosthetic and orthotic care, near you. If you have questions about insurance, appointment scheduling or anything in between, simply call 866-319-6762 or select the location nearest to you for contact information.